More than likely you’ve either had diagnostic imaging taken or have heard of X-rays, MRIs, and/or CT scans. These tests are great tools that provide medical professionals more insight and knowledge into the human body, allowing them to make more accurate diagnoses and choose the ideal treatment plan. Although all of these tools are used for diagnostic imaging, each one uses different techniques, providing varying levels of detail.
X-ray
X-rays are one of, if not the fastest and most accessible, forms of diagnostic imaging, commonly used as a first-line tool. It creates a 2D image by sending radiation through the body. How does this work? Dense areas of higher level of calcium (bones) block the radiation, leaving the image to appear white or transparent, while soft tissues (muscle, tendons, ligaments, etc.) allow the radiation to pass through and appear darkened, black, or grey. In some cases an X-ray may also look at internal structures with the use of barium sulfate, or dye, to make organs stand out more clearly. Although X-rays are great for seeing larger injuries to the bones, they don’t give a clear picture of more subtle injuries to bones or soft tissues.
Most commonly used for:
Fractures
Dislocations
Bone disease or degeneration
Pneumonia
Cancers and tumors
Computed Tomography Scan
A Computed Tomography scan, or CT scan, is yet another fast option for receiving diagnostic imaging, utilizing radiation and occasionally dye just like an X-ray. However, instead of providing a simplistic image, a CT scan provides a 3D image, giving a detailed computerized 360 degree view of bones, blood vessels, soft tissues, and organs. This makes a CT scan ideal for injuries related to trauma or in emergency situations.
Most commonly used for:
Trauma
Musculoskeletal disorders
Heart disease
Cancers
Appendicitis
Infectious diseases
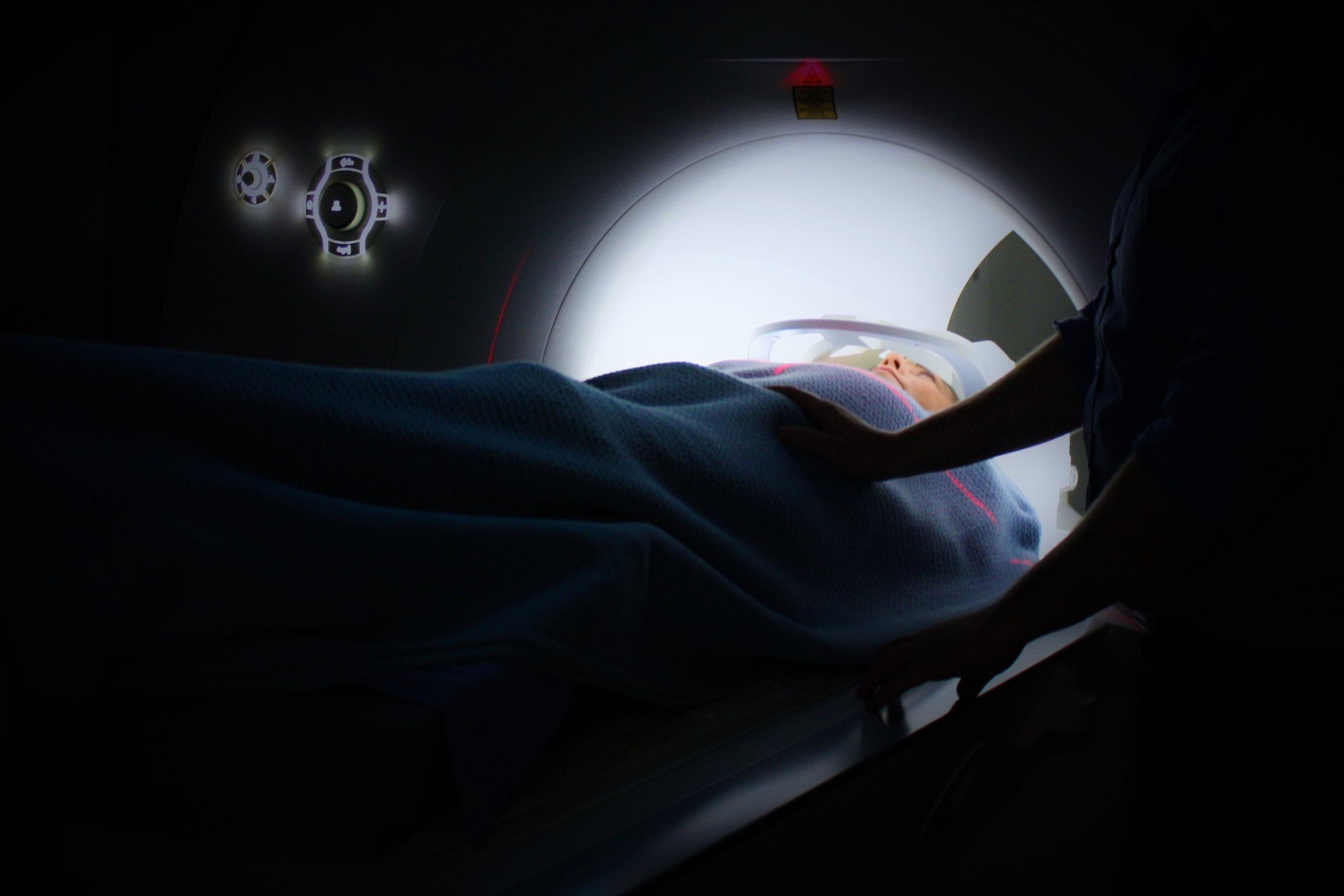
Magnetic Resonance Imaging
Magnetic Resonance Imaging, also known as an MRI, utilizes a powerful magnet and radio waves instead of radiation like X-rays and CT scans, creating highly detailed 3D cross section images, providing views of soft tissue, nerves, and blood vessels. An MRI can also give better contrast resolution for bones and soft tissues when compared to other diagnostic imaging. Due to the use of a powerful magnet some patients will not be able to have an MRI completed if they have metal implants, pacemakers, or other implanted devices.
Most commonly used for:
Injuries to ligaments, tendons, muscles (Meniscus, ACL, Achilles, Sprains/strains)
Cartilage damage
Joint injuries
Spinal injuries
Brain injuries